The heart rate is the rate of the pulse beat of the heart which pushes the blood through the circulatory system. It is being measured with special apparatus called manometer or there are newer versions of pressure measurements with digital pressure apparatus which shows the pressure and the pulse which is the heart rate.

The heart rate of a dog is also referred to as the pulse. It quantifies how many times a dog's heart beats in a minute and is recorded as beats per minute or BPM. A dog's heart pumps blood throughout the rest of the body and can be felt by a dog owner by placing a hand over their dog's heart. For most men and women, 60 to 100 beats per minute (bpm) is normal, according to the American Heart Association (AHA). In general, having a lower resting heart rate is generally healthier.
To understand the origin of pulse and heart rate, it is important to know the circulatory system and its parts. The heart is the main organ which is responsible for blood propulsion through the system. From this point, there are small and large circulation circles which are in charge of blood oxygenation and blood transmission to the body. The small circulation goes from the right atrium into the right ventricle and into the lungs via the pulmonary artery. This name for pulmonary artery is opposite from its function since it carries the vein blood or the deoxygenated one. It gets into the lungs and inside the alveoli, the oxygen is being submerged into the blood. From there, the big circulation occurs, where the oxygenated blood goes through the pulmonary veins into the left atrium and into the left ventricle. From the left heart, the blood goes through the aorta into the body where it gets used for body metabolism.
The pulse is the process of the blood getting inside the arteries by which it pushes the artery’s wall and it’s being transmitted to the manometer. Pulses can be felt all throughout the body, from the radial artery to the carotid artery, femoral artery, popliteal artery, brachial artery, tibial posterior and dorsal pedis artery. These are the most common arteries where you can feel the pulse.
What Is the Normal Rest Heart Rate?
A normal resting heart rate is being measured while being still, calm and sitting or lying in bed. It is best to measure in the morning in the bed or after you have been calm for at least ten minutes so your heart can slow down its rhythm to the appropriate rate.
How to Measure Normal Heart Rate?
You should first sit or lay down and have a few minutes of rest. Then, find one of the places where you can feel the pulse like we mentioned above. If you measure yourself, you can find the radial artery by placing your index finger and tour middle finger at the inside part of your wrist bellow your thumb. With your thumb below the wrist, you should secure the grip while holding your hand with your other two fingers above. If you are at the right spot, you should feel the pulse. When you have found the artery, use your watch to look at the seconds and count for pulse beats for 10 seconds. Multiply the number of pulses counted by 6 and you should get the pulse rate per minute since you have 60 seconds.
Pulse rate = ______ x 6 = ______beats/min.
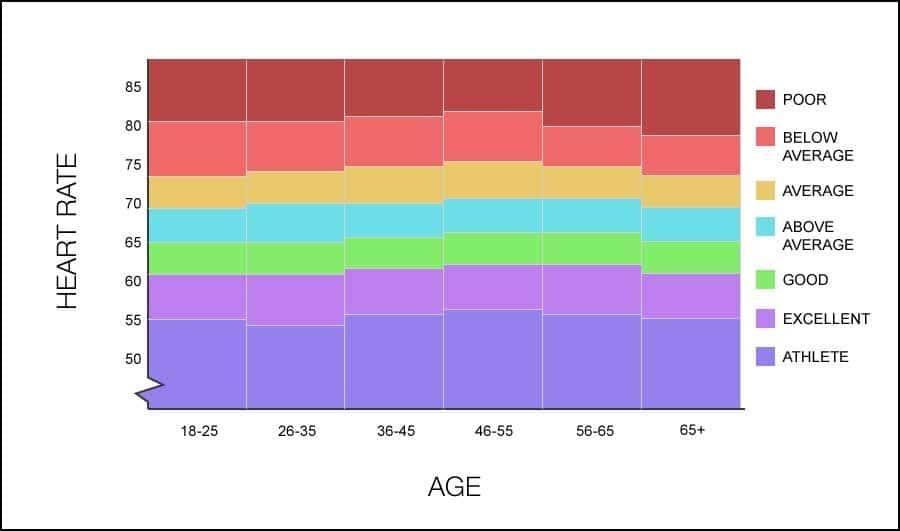
There are some differences for pulse rate among adults, children, and athletes. Here is the chart below. For the newborns and children, the pulse is faster and can get up to 160 beats per minute. As they grow, it goes down and it is from 60 to 100 from the age of 12. The athletes are known to have slow heart rate due to their training where they can have from 40 to 60 beats per second and this is considered normal due to circumstances.
Factor Which Can Influence Normal Heart Rate
There are some situations where your heart may slow down or speed up due to the activity of your body, stress, beverage consumption, etc. Here are some examples.
Normal Heart Pulse For Adults
Fast Pulse Rate
- Fever or some kind of flu
- Exercise and any kind of activity
- Anemia
- Alcohol consumption
- Stress
- Caffeine, tobacco, diet pills, amphetamines
- Hyperactivity of the thyroid gland
- Some kind of heart disease
- Some drugs that can stimulate the heart rate.
Slow Pulse Rate
- Trained people, athletes
- Hypothyroidism which is the name for inactive thyroid gland or an underactive one
- Heart failure or some other heart disease
Heart Rate During Exercise
There are two terms you should be familiar with, especially if you want to get the best out of your fitness. The maximum heart rate is the highest heart rate which is achieved when you are extremely active. This can be measured with the following formula:
220 – (your age) = maximum heart rate
Target heart rate is the optimal heart rate during exercise which targets your heart activity between 60 to 80%. This reduces the risk of injury and gets the best results at losing weight. If your heart rate is above 85% of your maximum heart rate, you are at risk of injury, either cardiovascular or orthopedic one.
Normal Maximum and Target Heart Rate
It depends on the person’s age. The moderate activity uses from 50-69% of maximum heart rate, while the intense workout can get up to 90% of maximum heart rate. Find your age in the chart and your best maximum and target heart rate.
Chart No. 2
How to Get at Target Heart Rate?
While you’re exercising, stop and count your pulse. This time, count it for 15 seconds. You can check at your carotid artery or radial artery. When you get the number of beats, multiple by 4 to calculate your pulse per minute. Then, put your age in the maximum heart rate formula and count your maximum heart rate. Then multiple 0.85 with the number you’ve got, and you will have 85% of maximum heart rate which is the target heart rate. If you’re over that number, try to slow down and adjust the intensity of your workout.
During evaluation, conduct the primary assessment, secondary assessment, and diagnostic tests. If at any time a condition is determined to be life-threatening, intervene immediately.
Normal Pulse Rate For Women 65
Primary Assessment
Assessment | Assessment Techniques | Abnormal Findings | Interventions |
A – Airway | Observe for movement of the chest or abdomen; Listen to the chest for breath sounds | Obstructed but maintainable | Keep airway open by head tilt/chin lift |
Obstructed and cannot be opened with simple interventions | Keep airway open using advanced interventions | ||
B – Breathing | Rate | <10 or >60 = Abnormal (apnea, bradypnea, tachypnea) | Immediate respiratory intervention required |
Effort | Nasal flaring, head bobbing, seesaw respirations, retractions | Immediate respiratory intervention required | |
Chest or abdominal expansion | Asymmetrical or no chest movement | Immediate respiratory intervention required | |
Breath sounds | Stridor, grunting, wheezing, rales, rhonchi | Immediate respiratory intervention required | |
Oxygen saturation (O2 sat) | <94% on room air <90% at any time | Supplemental oxygen Advanced airway | |
C – Circulation | Heart rate | Bradycardia | Bradycardia Algorithm |
Tachycardia | Tachycardia Algorithm | ||
Absent | Cardiac Arrest Algorithm | ||
Peripheral pulses (radial, posterior tibial, dorsalis pedis) | Diminished or absent | Close monitoring | |
Central pulses (femoral, brachial, carotid, and axillary) | Diminished or absent | Management of Pediatric Shock | |
Capillary refill | >2 seconds | Management of Pediatric Shock | |
Skin color/temperature | Pale mucous membranes | Management of Pediatric Shock | |
Central cyanosis | Immediate respiratory intervention required | ||
Peripheral cyanosis | Management of Pediatric Shock | ||
Blood pressure | Outside normal range for age | Management of Pediatric Shock | |
D – Disability | AVPU Scale | Alert – Awake, active, responsive to parents (normal) Uoice – Responds only to voice Pain – Responds only to pain Unresponsive – Not responsive | Monitor and consult neurologist |
Glasgow Coma Scale | Pediatric Glasgow Coma Scale | ||
Pupils | Unequal or non-reactive | ||
E – Exposure | General evaluation | Signs of bleeding, burns, trauma, petechiae, and purpura | Management of Pediatric Shock |
Table 3: Primary Assessment Model
Use the Primary Assessment to evaluate the child using vital signs and an ABCDE model:
A – Airway
Head tilt-chin lift and jaw thrust may be used to open the airway quickly and without the use of an advanced airway. The jaw thrust maneuver is preferred when a cervical spine injury is suspected or cannot be ruled out.
Advanced interventions for maintaining a patent airway may include:
- Laryngeal mask airway (LMA)
- Endotracheal (ET) intubation
- Continuous positive airway pressure (CPAP)
- Foreign body removal if one can be visualized
- Cricothyrotomy in which a surgical opening is made into the trachea.
Normal Heart Pulse For Women
B – Breathing
The child’s respiratory rate is an important assessment that should be made early in the primary assessment process. The clinician must be aware of normal respiratory ranges by age:
Age Category | Age Range | Normal Respiratory Rate |
Infant | 0-12 months | 30-60 per minute |
Toddler | 1-3 years | 24-40 per minute |
Preschooler | 4-5 years | 22-34 per minute |
School age | 6-12 years | 18-30 per minute |
Adolescent | 13-18 years | 12-16 per minute |
Table 4: Normal Respiratory Rates
A respiratory rate that is consistently below 10 or above 60 breaths per minute indicates a problem that needs immediate attention. Periodic breathing is not unusual in infants; therefore, you may have to spend more time observing the infant’s breathing to determine true bradypnea or tachypnea. Nasal flaring and retractions indicate increased work of breathing. Head bobbling or seesaw respirations are potential signs of impending deterioration. Likewise, slow and/or irregular breathing suggest imminent respiratory arrest.
C – Circulation
The child’s heart rate is another important assessment that should be made in the primary assessment. The normal heart rates by age are:
Age Category | Age Range | Normal Heart Rate |
Newborn | 0-3 months | 80-205 per minute |
Infant/young child | 4 months to 2 years | 75-190 per minute |
Child/school age | 2-10 years | 60-140 per minute |
Older child/ adolescent | Over 10 years | 50-100 per minute |
Normal Heart Pulse Rate
Table 5: Normal Heart Rates
The child’s blood pressure should be another part of the primary assessment. Normal blood pressures by age range are:
Age Category | Age Range | Systolic Blood Pressure | Diastolic Blood Pressure | Abnormally Low |
Systolic Pressure | 1 Day | 60-76 | 30-45 | <60 |
Neonate | 4 Days | 67-84 | 35-53 | <60 |
Infant | To 1 month | 73-94 | 36-56 | <70 |
Infant | 1-3 months | 78-103 | 44-65 | <70 |
Infant | 4-6 months | 82-105 | 46-68 | <70 |
Infant | 7-12 months | 67-104 | 20-60 | <70 + (age in years x 2) |
Preschool | 2-6 years | 70-106 | 25-65 | <70 + (age in years x 2) |
School Age | 7-14 years | 79-115 | 38-78 | <70 + (age in years x 2) |
Adolescent | 15-18 years | 93-131 | 45-85 | <90 |
Table 6: Normal Blood Pressure
D – Disability
Normal Heart Pulse In Neck
One of the assessments of level of consciousness in a child is the Pediatric Glasgow Coma Scale (GCS).
Response | Score | Verbal Child | Pre-Verbal Child |
Eye opening | 4 3 2 1 | Spontaneously To verbal command To pain None | Spontaneously To speech To pain None |
Verbal response | 5 4 3 2 1 | Oriented and talking Confused but talking Inappropriate words Sounds only None | Cooing and babbling Crying and irritable Crying with pain only Moaning with pain only None |
Motor response | 6 5 4 3 2 1 | Obeys commands Localizes with pain Flexion and withdrawal Abnormal flexion Abnormal extension None | Spontaneous movement Withdraws when touched Withdraws with pain Abnormal flexion Abnormal extension None |
Total Possible Score | 3-15 |
Table 7: Pediatric Glasgow Coma Scale
When there is a suspected or known head injury, a GCS score of 13 to 15 is considered mild, 9 to 12 is moderate, and 3 to 8 is severe. In intubated or sedated children, motor response provides the most important information. The lower the motor response score, the more serious the deficit/injury.
E – Exposure
If the provider finds any abnormal symptoms in this category they should assess and treat the child for shock (see Unit Seven: Management of Pediatric Shock, particularly Interventions for Initial Management of Shock). During the primary assessment, if the child is stable and does not have a potentially life-threatening problem, continue with the secondary assessment.
